Why is menopause still so stigmatized? Can’t we just talk about it like any other stage of life?
The stigma around menopause has been building for a long time.
Until about 100 years ago, there was very little medical information on menopause and many believed that menopause was a sign of menstruators' hysteria–a once diagnosed disorder.
This ideology that it was scary, problematic and something to be kept hidden was maintained throughout the years as societies remained uninformed about the menopause. In turn, the stigma persisted.
Thank goodness for brands like Alloy!

Alloy has come onto the scene to provide treatments, answers, and bust some myths about menopause. You should probably start thinking about these questions, regardless of how old you are!
Keep reading to find out the symptoms of menopause, what happens before, during and after menopause, and to unpack some menopause stereotypes.
All answers are verified by Alloy’s Chief Medical Officer, Dr. Sharon Malone MD, FACOG CNMP
On a medical level, what is menopause?
Menopause, simply put, is a biological process that marks the permanent end of a person’s ability to reproduce and the hormonal changes that ensue after.
The cause of a natural menopause is not just “running out of eggs” but the aging of the female ovaries. Eggs and the hormones that are normally produced during the menstrual cycle are functionally depleted at menopause.
The scientific breakdown is that the ovaries cease their production of estrogen, which is not simply a sex hormone but also has great impact on cells throughout the body. Estrogen is critical in hydrating cells, producing collagen, building bone mass, mitigating inflammation, and many other functions (hence the common symptoms of menopause which we’ll get into shortly!)
Menopause begins with the final menstrual period and is confirmed by twelve consecutive months of no periods. Menopause can also be induced by the surgical removal of the ovaries, chemotherapy or genetic factors well in advance of the average age of 51.
When does menopause start and how long does menopause last?

The average age for entering menopause is 51.
More broadly, for people in North America, menopause will typically come about between ages 40 and 58. Often, the age at which someone reaches menopause is the same as other close relatives (parents or siblings).
Before menopause, there is a phase called perimenopause, which literally means “around the menopause.” The differentiation of the phases is because menopause marks the end of fertility and means a persistent low level of hormones, while perimenopause is characterized more by the extreme fluctuations in hormones.
Perimenopause can last anywhere from 4 to10 years prior to the last menstrual period, and it is often during this phase that people are most symptomatic. The menstrual cycle typically shortens, coming too early, lasting too long, becoming heavier or lighter, before eventually becoming less frequent. Once the cycles become less frequent, you are typically closer to the final menstrual period.
Menopause is confirmed when you have gone twelve consecutive months without a period.
Fun fact:
Before 1900, the average life expectancy of someone with a uterus was 51! So most menstruators did not have to live for very long without estrogen.
But, now that the average life expectancy is closer to 80, and menstruators are living 30 to 40 years without estrogen, while they are still expected (and expect themselves) to work, take care of their families, take care of their aging parents, and have a social life, all without slowing down!
What menopause symptoms should I be looking out for?
-
Many people experience Genitourinary Syndrome of Menopause (aka the thinning of the vagina, which used to be referred to as vaginal atrophy), resulting in symptoms of vaginal dryness, itching, and often dyspareunia or painful intercourse.
-
Joint pain, breast pain and tenderness, and menstrual migraines can worsen around perimenopause.
-
Sleep problems such as insomnia, are known to increase the chances of Restless Leg Syndrome (RLS). While RLS is linked to menopause, menopause is not a cause of RLS.
-
Some folks may experience mood swings, anxiety and/or depression which may be new and frightening, but are not unusual during perimenopause. The decision to treat these symptoms should be made the same way as in any other phase of your life. Depression or anxiety that is interfering with your life or your ability to function should be addressed not simply tolerated.
-
Weight gain is often related to menopause due to lifestyle, hormonal imbalances, genetics, or a combination of those factors.
The symptoms that we associate most with menopause, such as hot flashes, mood swings and sleeplessness, actually start during the perimenopause and can persist for months to years after the final menstrual period.
Is menopause painful?

Yes and no.
People who have been plagued by painful periods, endometriosis and menstrual migraines can experience a welcome relief from many of these symptoms.
However, some people notice an increase in joint pains, painful sex and vulvar itching and burning at menopause. Most often, the aches and pains (even those unrelated to intercourse) can be reduced with treatment.
Pain caused by menopause does not need to have an impact on your quality of life, and, most importantly, can be addressed by either systemic or topical hormones.
If you are worried about pain you are experiencing, have a chat with a doctor.
Remember, menopause is inevitable. Suffering doesn’t have to be.
How should I explain menopause to my 9 year old?
We’d suggest something like this…
“Menopause is the time of life when the ability to naturally have a baby is over. In other words, no more chances for a younger sibling.To back track a bit so you have more understanding, menopause is a normal phase of a person’s reproductive life. It’s not just the end of things, but the beginning of a new phase of life that can be every bit as productive and vibrant as any other.”
It may be helpful for a 9 year old to understand the symptoms that may affect the mood of the person in their life going through menopause.
They should understand that the sometimes unexplained tearfulness, rage and sweating is not due to anything they have done, but is typically associated with the change in hormones. You could explain it similar to them getting a cold, when they’re a little extra sleepy and may feel hot or cold and need to change clothes back and forth to meet their body’s temperature.
Can some people not experience menopause?
Every person who, at one time, got a period will experience menopause, although not everyone will experience the same symptoms.
Symptoms can evolve over time as well, so just because you don’t experience symptoms at 51, for example, doesn’t mean you will not develop symptoms later on.
How is HRT used to treat menopause symptoms?
Symptoms like vaginal dryness, frequent UTIs, hot flashes, and insomnia from hot flashes are all reasons HRT (aka Hormone Replacement Therapy) can be used.
Hormone therapy is the most effective treatment for the symptoms of menopause. The FDA approved indications for hormone therapy are as follows:
- relief of vasomotor symptoms (hot flashes)
- treatment of vulvar and vaginal symptoms (Genitourinary Syndrome of Menopause)
- prevention of osteoporosis
Systemic hormone therapy also reduces the risk of developing Type 2 diabetes. In addition, those who start therapy between the ages of 50 and 60 have a 30% decrease in the risk of dying from all causes.
If you have a uterus, HRT consists of estrogen and a progestin to protect the uterine lining from cancer. If you do not have a uterus (usually due to hysterectomy), you only need estrogen. People who take estrogen not only have a 30% lower risk of developing breast cancer but also have a 30% lower risk of dying from all causes than nonusers.
For those with a uterus, both estrogen and progestin are used. These hormones can be bioidentical (the same hormone as made by the ovaries during a normal cycle) or non bioidentical or synthetic. Both are equally effective in relieving the symptoms of menopause, however, there is increasing evidence that bioidentical progesterone has fewer side effects and is less likely to increase the risk of breast cancer and blood clots. Alloy uses bioidentical estrogen and progesterone.
What can cause hot flashes other than menopause?

One of the most common reasons for developing hot flashes is an overactive thyroid. This is a simple diagnosis to make. A blood test (TSH and thyroid function) can rule out thyroid issues.
Hot flashes can also be a side effect of certain medications. Check with your doctor or pharmacist to see if the medications you are on can be contributing to new onset hot flashes.
Weight gain is also another contributor to heat intolerance. The heat intolerance associated with excess weight is typically more global. However, small amounts of physical activity can trigger sweating and feelings of intense heat.
The distinction between hot flashes and heat intolerance is often a matter of duration. Hot flashes typically have an abrupt onset and last less than five minutes.
Is it common to experience bladder leakage after menopause?

Bladder issues are extremely common after menopause.
Up to 80% of menpausal people experience urinary frequency or urgency at some time during menopause.
The vagina and the bladder are estrogen-sensitive tissues, so, the lack of estrogen after menopause compromises their normal function.
What are the risks of an early or premature menopause?
First, let’s go over a few definitions.
- Early menopause occurs when a person has had their final menstrual period before the age of 45.
- Premature menopause is when menopause occurs before the age of 40.
This is an important distinction because those who have early and premature menopause are at the higher risk for developing cardiovascular disease, Alzheimer’s disease, osteoporosis and having a shorter overall life expectancy.
Early or premature menopause can be the result of genetics, chemotherapy, or surgical removal of the ovaries. Sometimes a temporary menopause can be induced by certain medications used to treat endometriosis or shrink fibroids prior to surgery.
The difference between medically induced menopause and surgical or natural, early menopause is that the medical or chemotherapy induced menopause may not be permanent. That is why it is always important to confirm twelve months of no periods after the medication or treatments have been stopped.
And while pregnancy is not possible after surgery or natural menopause, it can occur after chemotherapy induced, or medically induced menopause.
Seek out a certified menopause practitioner for help finding information about your options when undergoing induced menopause.
What is post-menopause?

Post-menopause is what we generally consider “menopause”.
Once a person is in menopause, they are in menopause forever.
However, post-menopause simply refers to the period of time that starts twelve months after the final menstrual period and lasts a lifetime. For most people this phase lasts for over thirty years.
Can periods restart after menopause and is there a possibility of post-menopause pregnancy?
Typically, no. Regular menstrual periods do not restart after menopause unless the menopause is induced by medication or chemotherapy.
Since the fundamental part of menopause is a permanent lack of fertility, the only way a pregnancy can occur is with donor eggs.
Do men go through menopause?

Trans men who have functioning ovaries will go through menopause.
Trans men who have opted to have their ovaries removed will also go through a surgical (and abrupt) menopause.
However, if trans men are taking testosterone, they are less likely to be symptomatic.
Otherwise, cis men also go through hormonal changes to do with testosterone.
Some people have asked how to increase sex drive during menopause. What is the correlation between sex drive and menopause?
The correlation is hormones.
The ovaries make estrogen, progesterone and testosterone during the reproductive cycle.
Although estrogen and progesterone are important in ovulation and maintenance of pregnancy, testosterone produced at mid-cycle plays a big role in sex drive.
At menopause, not only do the estrogen and progesterone levels fall off a cliff – but so does testosterone. In fact, testosterone levels start to decline more than a decade before the last menstrual period.
For people who are bothered by this natural decline in sex drive, testosterone supplementation can be considered.
Because of the side effects of testosterone, (such as facial hair growth, male pattern baldness, deepening of the voice (irreversible), acne and enlargement of the clitoris), careful monitoring of the dose is key.
Have more questions about menopause? Looking for solutions to your symptoms?

Check out Alloy, who will help you to feel FANTASTIC, even as you go through menopause.
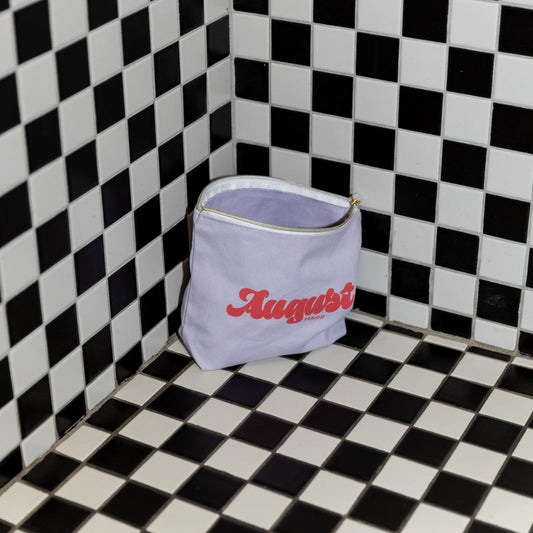
Looking for liners to get you through those menopausal years of irregular periods? Consider August’s 100% organic cotton option!
Stay tuned all month long for #BeyondMyPeriod stories from our communities being shared to both of our instagrams! @myalloy & @itsaugust